Human organoids, tiny organ-like structures grown in the laboratory, can be used to identify potential COVID-19 drugs in an automated, high-throughput fashion, according to a team led by investigators from Weill Cornell Medicine and NewYork-Presbyterian.
The study, published Oct. 28 in Nature, used lung and colon organoids made from human pluripotent stem cells, which have the potential to become any cell type, to test about 1,200 drugs for their efficacy in blocking SARS-CoV-2 infection. They identified several that appeared to be effective, one of which is already being tested in a clinical trial for COVID-19.
“This study demonstrates that you can use organoids derived from human pluripotent stem cells as a platform to discover drugs that block SARS-CoV-2 infection or progression of COVID-19,” said co-senior author Dr. Todd Evans, the Peter I. Pressman M.D. Professor of Surgery and associate dean for research at Weill Cornell Medicine. “Also, this platform can screen drugs that are already FDA-approved, which provides the added advantage of possibly being able to repurpose drugs that we already know are safe in patients, and therefore have the potential to move quickly into clinical trials.”
As the COVID-19 pandemic persists around the world, researchers continue to look for better ways to treat the effects of the disease. Many drugs that initially seemed promising ultimately were found to be disappointing in patients. And scientists still have very few good lab models of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection that can be used to evaluate potential new treatments.
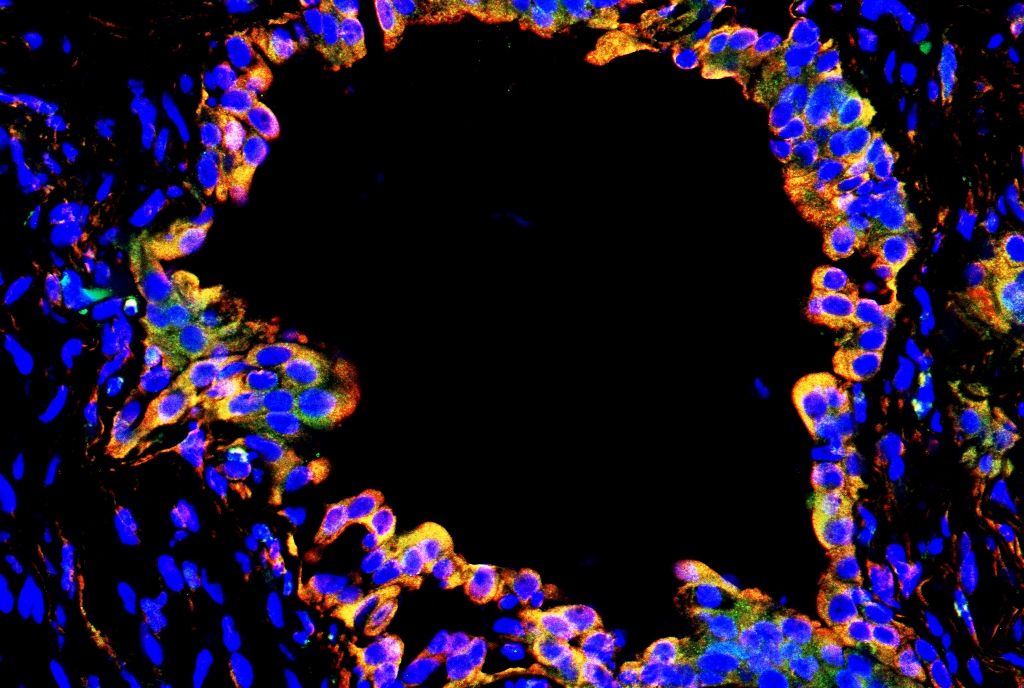
The organoids were developed in the laboratory of co-senior author Dr. Shuibing Chen, the Kilts Family Associate Professor of Surgery and an associate professor of chemical biology in surgery and of chemical biology in biochemistry at Weill Cornell Medicine. The team focused on two types of organoids, which contain lung alveolar type II cells and colonic enterocytes, respectively. These are two kinds of cells known to be widely infected in people with COVID-19, and these infections are associated with worse patient outcomes, according to Dr. Evans. The team had previously published research using liver and pancreas organoids to study the relationship between COVID-19 and diabetes.
“These organoid models are significant because they mirror what is seen when these types of cells are infected in patients with COVID-19,” Dr. Chen said. For example, some of the genes that were active in the organoids were the same ones that become active in patients experiencing cytokine storm—one of the most severe effects of COVID-19.
“We also showed that we can transplant these human organoids into a mouse, giving us a model to evaluate the efficacy of different compounds in human cells in a whole animal context,” Dr. Chen said. The organoids were infected with a pseudovirus—a modified version of SARS-CoV-2—as well as the active virus.
She adds that, to her knowledge, this is the first time organoids have been used as part of a high-throughput screening platform for any purpose on a broad scale.
The team focused on evaluating drugs that are already approved by the U.S. Food and Drug Administration for other diseases, so they could be more easily repurposed and moved into clinical trials quickly. They identified three promising compounds: imatinib (Gleevec), a targeted cancer drug; mycophenolic acid, an immunosuppressive medication; and quinacrine dihydrochloride, which is used to treat malaria as well as some autoimmune disorders. Their findings provide the first experimental justification for clinical trials recently initiated to evaluate imatinib in people with severe COVID-19.
“This was an unbiased screen that was looking for activity against infection,” said co-senior author Dr. Robert Schwartz, assistant professor of medicine in the Division of Gastroenterology and Hepatology at Weill Cornell Medicine and a hepatologist at NewYork-Presbyterian/Weill Cornell Medical Center. This means the researchers cast a wide net, rather than looking for drugs that would have particular activities. “We don’t know why this particular cancer drug would be effective against COVID-19, and that’s something we plan to study. These organoids are also a really useful research tool for trying to understand more about SARS-CoV-2 biology,” he said.
Dr. Schwartz added that because organoids can be made for every human organ type, this screening method could help to identify drugs that treat numerous harmful effects of COVID-19 disease. “If in fact we find the same drugs keep coming up, that’s a hopeful sign that they could be effective for treating systemic infections,” he said.
The researchers emphasized the collaborative nature of this project, which brought together not only five different labs at Weill Cornell Medicine but also scientists from Columbia University, the Icahn School of Medicine at Mount Sinai, and from outside New York City as well. “In some ways this pandemic has brought us together,” Dr. Evans said. “We are all laser-focused on this problem that acutely needs solving."